πίσω
πίσω
COPYRIGHT © by Michaelidou Maria
Dr. Maria Michailidou
General Considerations
Ankylosing spondylitis is regarded as the prototype of the spondyloarthropathies. Axial skeletal involvement predominates in ankylosing spondylitis, which invariably involves the sacroiliac joints and typically presents with the insidious onset of inflammatory low back pain during late adolescence or early adulthood. Onset of symptoms after the age of 40 is uncommon.
Although environmental factors are important in the development of ankylosing spondylitis,
the environmental triggers appear to be ubiquitous, and genetic background is the
major determinant of susceptibility to ankylosing spondylitis. The only known susceptibility
gene, HLA-
The disease course varies considerably, ranging from mild disease with little impact
on functional status to severe disease that produces substantial disability. The
extent of spinal involvement is a major determinant of the impact of the disease
on functional status. Unfortunately, there are no reliable predictors of long-
Clinical Findings
Symptoms and Signs in ankylosing spondylitis
Axial Spine
The typical presenting symptom in ankylosing spondylitis is the insidious onset of inflammatory low back pain due to sacroiliitis. The pain is dull and located in the lower lumbar regions, although some describe a deep alternating buttock pain. The characteristic inflammatory nature of the pain differentiates it from mechanical back pain; most notably, the pain worsens with rest, improves with activity, and is accompanied by morning stiffness that lasts 30 minutes or longer. Patients often describe awakening from sleep and pacing in order to relieve nocturnal pain— a rare complaint in patients with mechanical back pain.
There may be few objective findings in patients with early disease, making diagnosis a challenge. Palpation and specific maneuvers can elicit pain in the sacroiliac joints, but these tests are relatively insensitive and nonspecific due to the number of other anatomic structures that overlap within the same area.
Involvement of the spine (spondylitis) is the major source of morbidity. Unlike rheumatoid arthritis, which only affects the cervical spine, ankylosing spondylitis can involve the lumbar, thoracic, and cervical spine. Over time the accumulation of pathologic changes can lead to loss of spinal mobility, particularly of the lumbar spine. The Schober test is the standard examination to assess impaired lumbar flexion. Two marks are made on the patient's back: one at the level of the sacral dimples (approximately at the fifth lumbar spinous process) and the other 10 cm above. The patient then bends forward as far as possible (ie, attempts to touch toes with knees extended), and the distance between the two marks is again measured. In normal individuals, the overlying skin will stretch to 15 cm; values less than this can be indicative of reduced lumbar mobility. Some clinicians prefer the modified Schober test in which marks are made 5 cm below and 10 cm above the sacral dimples; the distance between these marks increases from 15 cm to at least 20 cm with lumbar flexion. Reductions in lumbar lateral bending and rotation are also commonly observed. Spinal fusion results in irreversible impairments, but reductions in mobility also can be induced by pain or muscle spasm and, therefore, vary somewhat with time and treatment. With advancing disease, a characteristic posture often develops as the spine fuses in flexion, leading to loss of lumbar lordosis, exaggeration of thoracic kyphosis, an inability to extend the neck, and compensatory hip flexion deformities
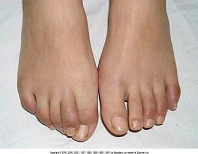
Peripheral Joint Manifestations
Peripheral arthritis, typically monarticular or asymmetric oligoarticular, develops
in approximately one-
Enthesitis
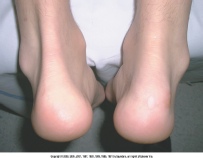
Involvement of insertion sites around the pelvis (the ischial tuberosities, iliac crests, and greater trochanters) is common and appears on radiographs as bony "whiskering" at these sites of attachment. Achilles tendinitis and enthesitis at the site of the insertion of the plantar fascia onto the calcaneus can cause unilateral or bilateral heel pain, although not as often as in reactive arthritis.
Ocular
The most common extra-
Other Organs
The majority of patients with ankylosing spondylitis have histologic evidence of
inflammation on biopsy specimens of the small or large bowel. These changes are asymptomatic
but may be of pathogenetic importance in view of the link between clinically overt
inflammatory bowel disease and spondyloarthropathy and the apparent importance of
colitis in the transgenic rat model of HLA-
Cardiac involvement in the form of ascending aortitis, aortic regurgitation, conduction
abnormalities, and myocardial disease occurs in approximately 10% of patients with
ankylosing spondylitis, and, like uveitis and axial disease, is strongly associated
with HLA-
Restriction in chest wall motion from enthesitis or bony fusion commonly produces mild impairment of pulmonary function; characteristic spirometry findings include a slight reduction of vital and total lung capacity and normal diffusion capacity. Most patients, however, are asymptomatic, and clinically significant pulmonary disease is uncommon. A rare pulmonary finding in ankylosing spondylitis is the development of apical fibrobullous disease that radiographically resembles reactivation of tuberculosis and that can become a site for bacterial or fungal infections.
Of the neurologic consequences of spondyloarthritis, the most important is spinal
fracture, which often goes unrecognized and leads to neurologic compromise in about
one-
Rare manifestations of the spondyloarthropathies include the late development of secondary amyloidosis. An association of ankylosing spondylitis with retroperitoneal fibrosis has been suggested.
Laboratory Findings in ankylosing sponylitis
Routine laboratory investigations often reveal a mild, normocytic, normochromic anemia,
reflective of chronic disease. Only about half of patients with active disease will
have elevations of the erythrocyte sedimentation rate or C-
No laboratory test is diagnostic of ankylosing spondylitis or the other spondyloarthropathies.
Inheritance of HLA-
Nonsteroidal Anti-
Almost all patients are prescribed at least one nonsteroidal anti-
Disease-
NSAIDs alone do not control the symptoms of many patients. Sulfasalazine has established efficacy in treating the peripheral arthritis of ankylosing spondylitis but does not appear to be of benefit for disease of the axial skeleton. The typical therapeutic dose is 2–3 g/d in divided doses. Methotrexate is sometimes used; the rationale for this is based mainly on its efficacy in rheumatoid arthritis, as controlled studies are lacking.
Intravenous bisphosphonates have recently been demonstrated to effectively treat
the pain and inflammation of both the peripheral and axial disease of spondyloarthropathy.
Pamidronate is typically given as a 30–60-
Etanercept and infliximab, both anti-
Other Pharmacologic Therapies
Systemic glucocorticoids are not commonly used and can worsen osteopenia. In certain
cases, intra-
Surgical Therapy
The deformities that result from extensive disease of the spine can lead to disabling decreases in the field of vision and ambulation. Corrective surgeries of spinal alignment, however, are major procedures and have limited indications. Typically, osteotomy with fixation is performed, with corrections of the lumbar spine being most common. Neurologic complications and perioperative mortality are not insignificant with these procedures.
Hip involvement requires artificial replacement in approximately 5% of patients with
ankylosing spondylitis. The outcome of total hip arthroplasty is good, with long-
ANKYLOSING SPONDYLITIS